Health
11 best foods to lower bad cholesterol (LDL)

Discover the best 11 foods to lower bad cholesterol (LDL).
Foods and ingredients that, incorporated into the diet, help us fight bad cholesterol.
Cholesterol is a molecule composed of fatty acids that, when found in excessive levels in the blood, can cause heart disease, which is why there is a general concern to lower cholesterol levels.
Exercise, maintaining a healthy weight, not smoking, and adding foods to lower bad cholesterol to the diet are the recommendations that doctors make to counteract this evil.
10 foods that help lower bad cholesterol
For cholesterol to be transported through the blood, it needs lipoproteins; When these are of low density and their levels are excessive, they accumulate in the circulatory system, blocking it, the so-called “bad cholesterol” appears.
On the other hand, if the lipoproteins are of high density, they transport the cholesterol that accumulates in the circulatory system and helps to eliminate it, it is the “good cholesterol”
What foods help lower bad cholesterol levels? Let’s see a few.
1. Oatmeal
It is the food par excellence in the mission of lowering bad cholesterol levels. It contains a fiber that, unlike other cereals, is soluble.
It is recommended to consume three grams of oats daily, and when cholesterol levels are not very high, in a few weeks they will drop considerably.
2. Apple
Eating an apple a day takes care of the arteries, as it reduces the absorption of the fact that other foods provide.
This fruit to a certain extent prevents cholesterol from adhering to the wall of the blood vessels thanks to the fact that it contains flavonoids.
It will also help you fight hypertension and not retain fluids. In short, regularly consuming apples is excellent for lowering blood cholesterol levels.
3. Flax and Chia Seeds
These seeds are a good source of omega 3 and studies show that their consumption reduces cholesterol between 6 and 13%. Chia seeds are also very rich in fiber and antioxidants.
They can be included in salads as the recommendation is that they be consumed without soaking.
4. Egg white
Contrary to the belief that eggs raise blood cholesterol levels, the fatty acids in egg whites help increase good cholesterol. Having two boiled egg whites for breakfast is one of the best food alternatives to lower bad cholesterol.
5. Vegetable oils
Sunflower, olive, or canola oil should substitute for oils of animal origin. These vegetable oils contain polyunsaturated fatty acids.
Accompanying salads or vegetables and fruits with these oils that help lower cholesterol levels is an excellent option.
6. Eggplant
Eggplant is a fruit that contains chlorogenic acid that helps prevent good cholesterol from oxidizing. It also works by absorbing cholesterol in the blood. It should be eaten cooked and whole without removing the skin or the seeds.
Eggplant is a powerful food to lower cholesterol levels; just cut it into large pieces, cook it and consume it to notice results in a short time.
7. Walnuts
Walnuts contain a type of omega 3 that not only increases good cholesterol and reduces bad cholesterol, but also promotes the elasticity of blood vessels, prevents blood clots, and lowers high blood pressure.
It is enough to consume 3 or 4 a day for this seed to lower cholesterol levels. But you should not eat too many, as they contain a lot of fat.
8. Legumes
These are effective foods to lower bad cholesterol because they are a source of soluble fiber that works like a broom, sweeping it away and then eliminating it along with the feces.
But it is not the only function of legumes. When fiber is working, the liver needs more cholesterol to produce more bile salts, thus reducing its concentration.
Lentils, beans, chickpeas, and beans should be consumed regularly to reduce bad cholesterol in the body.
9. Blueberries
These berries increase good cholesterol and reduce blood pressure, artery stiffness, and general inflammation. In general, they are considered an excellent food to take care of the heart and their consumption is excellent for lowering good cholesterol.
Blueberries can be consumed dried or fresh and in either form is food that lowers cholesterol levels.
10. Fatty fish
Faced with a high level of cholesterol in the blood, we must eliminate the consumption of red meat. A good substitute for these is fish such as mackerel, salmon, tuna, sardine, or trout. They can be cooked on the grill.
These foods are rich in omega 3, so they lower blood pressure, prevent blood clotting, and therefore lower total cholesterol.
11. Almonds and chocolate
The surprise on the list of foods that lower bad cholesterol is chocolate. The truth is that the exact combination of almonds and chocolates has proven to be heart-healthy.
Research-backed by the University of Pennsylvania has shown that 20 g of almonds along with ¼ cup of dark chocolate reduce low-density lipoproteins, thereby lowering bad cholesterol.
Health
Benefits of bay leaves and side effects

Table of Contents
Health
Serious side effects of metoprolol

- Discover the serious side effects of metoprolol.
- How does this medication work? What are its effects?
- Metoprolol belongs to the class of medications called beta-blockers. Metoprolol is used to treat high blood pressure and prevent symptoms of certain types of angina ( chest pain). It is also used to reduce the risk of death immediately after a heart attack. It works by reducing the needs of the heart during exercise.
- People who have had a heart attack take metoprolol to avoid having another heart attack. Metoprolol is often used in combination with other drugs that lower high blood pressure, such as diuretics (pills that increase urine output), when just one agent is not enough to control blood pressure.
- This medicine is available under various brand names or in different formulations, or both. A specific brand of this medication may not be available in all forms and may not have been approved for all of the conditions discussed here. Also, some forms of this medicine may not be used for all of the conditions mentioned in this article.
- Your doctor may have suggested this medication for a condition that is not listed in this Medication Information article. If you have not yet discussed this with your doctor, or if you are not sure why you are taking this medicine, consult your doctor. Do not stop taking this medicine without consulting your doctor first.
- Do not give this medicine to anyone, even someone who has the same symptoms as yours. This medicine could harm people for whom it was not prescribed.
- What forms does this medication come in?
- Apo-Metoprolol
- 25 mg
- Each white, oval, scored tablet, engraved “ME” over “25” on one side and “APO” on the other, contains 25 mg of metoprolol tartrate. Nonmedicinal ingredients: colloidal silica dioxide, croscarmellose sodium, lactose monohydrate, magnesium stearate, and microcrystalline cellulose.
- 50 mg
- Each white, round, scored tablet, engraved “APO” over “M50”, contains 50 mg of metoprolol tartrate. Nonmedicinal ingredients: colloidal silica dioxide, croscarmellose sodium, lactose, magnesium stearate, and microcrystalline cellulose.
- 100 mg
- Each white, round, scored tablet, debossed with “APO” over “M100”, contains 100 mg of metoprolol tartrate. Nonmedicinal ingredients: colloidal silica dioxide, croscarmellose sodium, lactose, magnesium stearate, and microcrystalline cellulose.
- Apo-Metoprolol (Type L)
- 50 mg
- Each pink, capsule-shaped, coated tablet, scored on one side and engraved “50” on the other, contains 50 mg of metoprolol. Nonmedicinal ingredients: carnauba wax, colloidal silica dioxide, croscarmellose sodium, D&C aluminum lake red No. 30, sun yellow aluminum lake, hydroxypropyl methylcellulose, lactose, magnesium stearate, microcrystalline cellulose, polyethylene glycol 3350, and sodium dioxide. titanium.
- 100 mg
- Each blue, capsule-shaped, coated tablet, scored on one side and engraved “100” on the other, contains 100 mg of metoprolol. Nonmedicinal ingredients: carnauba wax, colloidal silica dioxide, croscarmellose sodium, hydroxypropylmethylcellulose, indigotin aluminum lake (AD & C blue # 2), lactose, magnesium stearate, microcrystalline cellulose, polydextrose, polyethylene glycol 3350, and titanium dioxide.
- How should this medication be used?
- The usual maintenance dose of metoprolol ranges from 100 mg to 200 mg per day, however, this dose may be increased to 400 mg per day as needed to achieve symptom control. Immediate-release tablets are taken in 2 divided doses while slow-release tablets are taken once a day.
- This medication should be taken soon after a meal, but try to take it at the same time every day.
- Several factors can be taken into account in determining the dose a person needs: their weight, their health, and whether they are taking other medications. If your doctor has recommended a dose other than those listed here, do not change the way you are taking the medicine without consulting your doctor.
- This medicine must be taken exactly as your doctor has told you. If you miss a dose, take the medicine as soon as you notice the missed dose and resume treatment as soon as possible. If it is almost time for your next dose, skip the missed dose and go back to your usual dosing schedule. Do not use a double dose to make up for a missed dose. If you are unsure of what to do after missing a dose, ask your doctor or pharmacist for advice.
- Store this medication at room temperature, protect it from light and moisture, and keep it out of the reach of children.
- Do not dispose of medicines in the wastewater (eg not in the sink or in the toilet bowl) or with the household garbage. Ask your pharmacist how to dispose of unused or expired medicines.
- In which cases is this medication not recommended?
- Do not use this medicine under the following circumstances:
- a condition such as right ventricular failure caused by high blood pressure in the lungs;
- is allergic to metoprolol or any of the ingredients of the medication
- are allergic to other beta-blockers;
- anesthesia caused by an agent having a depressant effect on the myocardium (eg ether);
- a history of heart attack accompanied by:
- a heart rate of fewer than 45 beats per minute,
- severe heart block
- very low blood pressure
- moderate or severe heart failure.
- slow heartbeat caused by problems with the heart rhythm;
- severe heart block;
- cardiogenic shock;
- significant circulatory disorders;
- proven heart failure;
- the presence of asthma or other obstructive airway conditions (only when it comes to metoprolol in intravenous form);
- a disorder referred to as “sinus dysfunction syndrome”;
- have untreated pheochromocytoma (a tumor of the adrenal glands).
- What are the possible side effects of metoprolol
- Many medications can cause side effects. A side effect is an unwanted response to a drug when taken in normal doses. It can be mild or severe, temporary or permanent. The side effects listed below are not experienced by everyone who takes this medication. If you are concerned about side effects, discuss the risks and benefits of this medication with your doctor.
- At least 1% of people taking this medicine reported the following side effects. Many of these side effects can be managed and a few may go away on their own over time.
- Consult your doctor if you experience these side effects and if they are serious or bothersome. Your pharmacist may be able to give you advice on what to do if these side effects appear:
- changes in libido or sexual ability;
- constipation;
- diarrhea;
- pain or discomfort in the abdomen;
- dizziness or light-headedness when changing from sitting or lying down to standin
- fatigue or unusual weakness brought on by activity;
- fatigue;
- headaches;
- nausea;
- hair loss;
- weight gain;
- dreams giving a powerful sensation;
- dry mouth;
- increased sensitivity of the skin to solar radiation;
- increased sweating;
- sleep disturbances;
- vomitings.
- Most of the side effects listed below do not happen very often, but they could cause serious problems if you do not see your doctor or receive medical attention.
- Check with your doctor as soon as possible if any of the following side effects occur:
- slow heartbeat (especially less than 40 beats per minute);
- hearing changes;
- confusion;
- difficulty breathing or wheezing;
- back or joint pain;
- chest pain;
- hallucinations (the perception of phenomena that do not exist);
- tingling in the arms and legs.
- a feeling of coldness in the hands and feet;
- signs of depression (eg, lack of concentration, weight fluctuations, trouble sleeping, indifference to many activities, thoughts of suicide);
- signs of certain heart problems (e.g., increased or irregular heartbeat or pulse, chest pain, difficulty breathing, excessive fatigue, swelling of the feet, ankles, or part lower legs);
- signs of certain kidney problems (eg increased or reduced urine production, itching, nausea, vomiting, rash);
- signs of a bleeding disorder (e.g. unusual nosebleeds, bruising, blood in urine, cough with bloody sputum, bleeding gums, cuts that keep bleeding) ;
- signs of liver problems (eg, nausea, vomiting, diarrhea, loss of appetite, weight loss, yellowing of the skin or whites of the eyes, dark urine, pale stools );
- a flare-up of psoriasis (eg, red spots the size of a pinhead on the skin; red, scaly, or crusty skin);
- a feeling of numbness or tingling in the extremities;
- symptoms of low blood pressure (eg, dizziness, fatigue);
- vision changes (eg blurred vision, dry eye, eye pain).
- Stop taking the drug and seek immediate medical attention if there is a response such as :
- coldness, discoloration, or pain in the fingers or toes;
- symptoms of a serious allergic reaction (such as swelling of the face or swelling of the throat, hives, or difficulty breathing).
- Some people may experience side effects other than those listed. See your doctor if you notice any symptom that worries you while you are using this medicine.
- Are there other precautions or warnings?
- Before using any medication, be sure to tell your doctor about any medical conditions or allergies you may have, the medications you are using, and any other important facts about your health. Women should mention if they are pregnant or breastfeeding. These factors could influence how you should use this medicine.
- Respiratory disorders: In general, people with asthma, and certain other lung problems, should generally avoid taking beta-blockers such as metoprolol, as they can cause breathing difficulties. If you have breathing problems, and your doctor has prescribed metoprolol for you, it is probably in lower doses, and they will monitor you regularly while you are using this medicine. If you have breathing problems, talk to your doctor about how this medicine may affect your condition, how your condition affects the administration and effectiveness of this medicine, and whether medical supervision is needed. specific.
- Severe allergies: If you have allergies severe enough to cause anaphylaxis (a severe allergic reaction in which swelling of the face, lips, and throat makes it very difficult to breathe), talk to your doctor about what to do next. take if you have an allergic reaction. the use of metoprolol may make it more difficult to treat severe allergic reactions with epinephrine.
- Stopping the drug: People with heart disease who suddenly stop taking this drug may experience chest pain, irregular heartbeat, or a heart attack. If you have heart disease, do not stop taking this medication without consulting your doctor first. When this medication is to be stopped, it should be done gradually, under the supervision of your doctor.
- Diabetes: The signs associated with low blood sugar may be more difficult to see while you are taking metoprolol. People with diabetes may have a harder time regulating their blood sugar levels when taking this medicine. If you have diabetes, discuss with your doctor how this medication may affect your condition, how your condition affects the administration and effectiveness of this medicine, and whether medical supervision is needed. specific. You will be kept under medical supervision while taking this medicine and your doctor may need to adjust your doses of diabetes medicine.
- Dizziness or syncope: Metoprolol may cause side effects, including dizziness or fainting, soon after starting treatment. Do not drive a vehicle or do other potentially dangerous tasks until you know how this medicine works for you.
- Hyperthyroidism (high level of thyroid hormones): Metoprolol may mask the symptoms of a person with hyperthyroidism (high level of thyroid hormones).
- If you have hyperthyroidism, discuss with your doctor how this medication may affect your condition, how your condition affects the administration and effectiveness of this medicine, and whether it is appropriate to have it. specific medical surveillance. Stopping the medication suddenly could make this condition worse.
- Liver function: Liver disease or reduced liver function can cause this drug to build up in the body, causing side effects. If you have liver problems, talk to your doctor about how this medicine may affect your condition, how your condition affects the administration and effectiveness of this medicine, and whether medical supervision is needed. specific. Your doctor will monitor your liver function with regular blood tests while you are taking this medicine.
- If you notice symptoms of liver problems such as fatigue, feeling unwell, loss of appetite, nausea, yellowing of the skin or whites of the eyes, dark urine, pale stools, abdominal pain, or swelling and itching of the skin, contact your doctor immediately.
- Kidney function: Taking metoprolol may affect kidney function. Your doctor will take this into account in his monitoring and will adjust your dose as needed. If you have reduced kidney function or kidney disease, talk to your doctor about how this medicine may affect your condition, how your condition affects the administration, and how well this medicine works. , and the relevance of specific medical surveillance. If you notice swelling in your hands, feet, or face, an increase in your blood pressure, unusual muscle cramps, or a dark appearance of your urine, this medicine may be interfering with the proper function of your blood. kidneys.
- If you notice any of these symptoms, contact your doctor as soon as possible.
- Heart disease: Beta-blockers like metoprolol can worsen already present heart failure. It is essential to use metoprolol as prescribed by your doctor to reduce this risk. If you have a history of heart disease, discuss with your doctor how this medication may affect your condition, how your condition affects the administration and effectiveness of this medicine, and whether it is appropriate to use it. specific medical surveillance.
- Pheochromocytoma: This medicine may worsen the symptoms of pheochromocytoma (a tumor of the adrenal gland) if taken alone Talk to your doctor about how this medicine might affect your condition, how your condition affects your condition. administration and efficacy of this medicinal product, and the relevance of specific medical supervision.
- Surgery: If you are about to have surgery, tell all healthcare professionals who treat you that you are using metoprolol.
- Pregnancy: This medication should not be used during pregnancy unless the benefits outweigh the risks. If pregnancy occurs while you are using this medicine, contact your doctor immediately.
- Breast-feeding: This medicine passes into breast milk. If you use metoprolol while you are breastfeeding your baby may feel the effects. Check with your doctor to see if you should continue breastfeeding.
- Children: The safety and effectiveness of this medicine have not been established in children
- Seniors: Normal doses of metoprolol for adults may lower blood pressure more than expected. Lower doses may be necessary for the elderly.
- Can other agents interact with this medication?
- There may be an interaction between metoprolol and any of the following:
- abiraterone acetate;
- acetylcholine;
- anesthetic agents;
- alpha agonists (eg, clonidine, methyldopa);
- alcohol;
- aldesleukin;
- aliskiren;
- alpha1-blockers (eg doxazosin, prazosin, tamsulosin);
- amifostine;
- amiodarone;
- amphetamines (eg, dextroamphetamine, lisdexamfetamine);
- serotonin antagonists (antiemetic drugs; eg dolasetron, granisetron, ondansetron);
- tricyclic antidepressants (eg amitriptyline, clomipramine, desipramine, trimipramine);
- antihistamines (eg, cetirizine, doxylamine, diphenhydramine, hydroxyzine, loratadine, diphenhydramine);
- nonsteroidal anti-inflammatory drugs (NSAIDs) eg. ibuprofen, indomethacin, naproxen);
- antimalarials (e.g. chloroquine, hydroxychloroquine, mefloquine, quinine);
- antipsychotics (eg, chlorpromazine, clozapine, haloperidol, olanzapine, quetiapine, risperidone);
- asunaprevir;
- atomoxetine;
- other beta-blockers (eg, atenolol, pindolol, propranolol);
- azelastine;
- barbiturates (eg, butalbital, pentobarbital, phenobarbital);
- beta-agonists (anti-asthma medicines, eg salbutamol, salmeterol, formoterol);
- calcium channel blockers (eg, verapamil, diltiazem, nifedipine, amlodipine);
- angiotensin II receptor blockers (ARBs) eg. irbesartan, losartan);
- bortezomib;
- brimonidine;
- buprenorphine;
- bupropion;
- celecoxib;
- ceritinib;
- milk thistle;
- cholecalciferol;
- cimetidine;
- cinacalcet;
- clobazam;
- clotrimazole;
- cobicistat;
- cocaine;
- cyproterone;
- darifenacin;
- delavirdine;
- rye ergot derivatives (eg bromocriptine, ergotamine, methylergonovine);
- nitro derivatives (eg nitroglycerin, isosorbide dinitrate, isosorbide mononitrate);
- dextromethorphan;
- digoxin;
- dipyridamole;
- disopyramide;
- disulfiram;
- diuretics (pills to remove water; eg furosemide, hydrochlorothiazide);
- donepezil;
- doxorubicin;
- dronedarone;
- entacapone;
- epinephrine;
- grass pollen allergen extract;
- fentanyl;
- fingolimod;
- flecainide;
- floctafenine;
- galantamine;
- ginger;
- ginseng;
- guanfacine;
- imatinib;
- phosphodiesterase type 5 inhibitors (eg, sildenafil, tadalafil);
- proton pump inhibitors (eg, lansoprazole, omeprazole, rabeprazole);
- Angiotensin-Converting Enzyme Inhibitors (ACEIs) eg. captopril, ramipril);
- selective serotonin reuptake inhibitors (eg fluoxetine, paroxetine, sertraline);
- selective serotonin-norepinephrine reuptake inhibitors or SNRIs (eg, desvenlafaxine, duloxetine, venlafaxine);
- insulin;
- isoniazid;
- ketoconazole;
- lacosamide;
- lanreotide;
- levodopa;
- lidocaine;
- lomustine;
- cholesterol “statin” drugs (eg pravastatin, simvastatin);
- methacholine;
- methadone;
- methimazole;
- methoxsalen;
- methylphenidate;
- metoclopramide;
- midodrine;
- mifepristone;
- mirabegron;
- moclobemide;
- nefazodone;
- nevirapine;
- nilotinib;
- noradrenaline;
- octreotide;
- orphenadrine;
- oxybutynin;
- pasireotide;
- pazopanib;
- peginterferon alfa-2b;
- pentoxifylline;
- sodium phenylbutyrate;
- pilocarpine;
- pimozide;
- praziquantel;
- propafenone;
- quinidine;
- quinine;
- ranitidine;
- regorafenib;
- rifabutin;
- rifampin;
- rituximab;
- rivastigmine;
- ropinirole;
- sulfonylureas (eg gliclazide, glyburide, tolbutamide);
- temsirolimus;
- terbinafine;
- theophyllines (eg aminophylline, oxtriphylline, theophylline);
- ticagrelor;
- ticlopidine;
- tizanidine;
- tofacitinib;
- tolcapone;
- tranylcypromine;
- yohimbine.
- If you are taking any of the above medicines, please tell your doctor or pharmacist. In your case, your doctor may ask you to:
- stop taking any of the medications;
- replace one of the drugs with another;
- change the way you take one or both of the medicines.
- do not change anything at all.
- Interference of one medicine with another does not always mean that you stop taking one of them. Ask your doctor what to do with drug interactions.
- Drugs other than those listed above may interact with this drug. Tell your doctor everything you take, whether it is prescription or over-the-counter drugs and herbal remedies. Do not forget to mention any supplements you take. If you consume caffeine, alcohol, nicotine, or street drugs, you should tell your prescribing doctor since these substances can affect the way many drugs work
Health
Side effects of too much cinnamon

Table of Contents
-

 Food1 year ago
Food1 year ago10 + Benefits of carrot juice and side effects
-

 Benefits4 months ago
Benefits4 months agoThe Benefits of Joining Gym Lumolog – Improve Your Fitness & Health
-

 Health1 year ago
Health1 year ago50 Super Healthy (And Very Often Cheap) Foods
-

 Health1 year ago
Health1 year ago5 Shocking health benefits of kinkeliba and side effects
-

 Food1 year ago
Food1 year ago8 shocking benefits of leek juice and side effects
-

 Health1 year ago
Health1 year agoBenefits of guava leaves Sensually
-
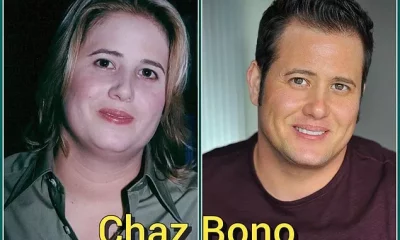
 Weight Loss1 year ago
Weight Loss1 year agoChaz Bono weight loss secret
-

 Health1 year ago
Health1 year ago15 Benefits of lipton tea and side effects












